Jump to:
- Arthrodesis (Fusion)
- Ligament Reconstruction and Tendon Interposition (LRTI)
- Total Joint Arthroplasty
- Trapeziectomy
What is thumb arthritis?
Our thumbs are used in almost every single daily task. In fact, without our thumbs we would lose over 40% of our hand function. Imagine trying to grasp a mug, open a door handle, use your cellphone, or get dressed without the use of your thumb. Those tasks would be both difficult and awkward without our thumbs because they require some form of pinch and grasp, a movement made possible by our thumb.
The thumb’s great mobility comes with decreased stability. The opposable feature is great for our daily tasks, but is highly susceptible to repetitive movements and cartilage breakdown. This leaves it susceptible to arthritis and arthritis pain.
Why would someone need surgery?
As the joint cartilage breaks down, it can become painful and very annoying. Over time, the ligaments supporting the joint can loosen, adding increasing pressure to the articular cartilage.
The joint can also collapse as the ligament tension weans or as the inflammatory response of rheumatoid arthritis affects the surrounding joint tissue.
Initially, pain may only be tied to activity or making a pinch. But as the arthritis progresses, pain can be felt almost all the time and at rest.
Conservative measures like exercises, joint protection, activity modification, and thumb splints are the first line of defense for managing thumb arthritis. However, pain may persist despite implementation of these conservative strategies.
To try some hand exercises that can help check out daily hand exercises for arthritis or if you’d like to know which thumb support is right for you read our post: What is the Best Thumb Support for My Arthritis?
If you’ve tried all conservative measures with insufficient results, surgery might be the right option.
Four Types of Thumb Surgery for Arthritis
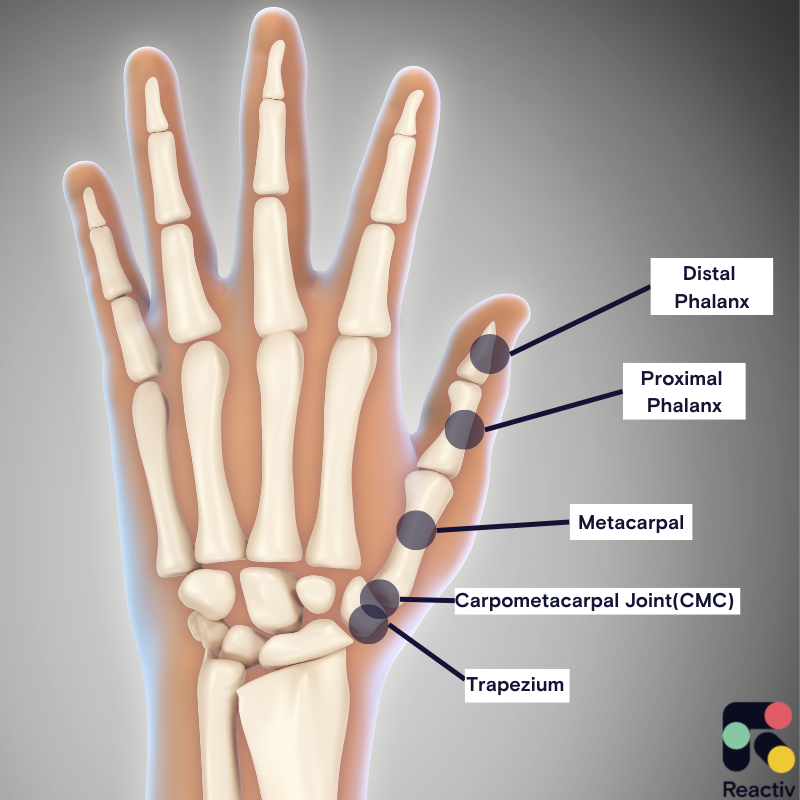
Your thumb is made up of three bones, the metacarpal, proximal phalanx, and the distal phalanx.
The metacarpal bone forms a joint with your carpal bone called the trapezium. The joint between the trapezium and the metacarpal bone is called the carpometacarpal joint (CMC). You may also see it referred to as the basilar thumb joint, which is the same as the CMC.
Here are the four main types of surgeries linked with thumb arthritis:
- Arthrodesis (Fusion)
- Ligament Reconstruction and Tendon Interposition (LRTI)
- Total Joint Arthroplasty
- Trapeziectomy
Arthrodesis (Fusion)

Who is it for?
Arthrodesis or a thumb fusion is when the surgeon pins two bones together to limit movement completely in that joint. Typically, it is between the trapezium carpal bone and the carpometacarpal (CMC) joint, as depicted in the image above.
This may be beneficial for someone who is younger and requires a lot of manual work or repetitive pinching. For example, a carpenter whose job requires the use of a hammer.
It may also be necessary for someone with rheumatoid arthritis who may have already had thumb surgery but symptoms persist.
What is an arthrodesis?
In an arthrodesis of the thumb’s carpometacarpal (CMC) joint, the metacarpal bone is fused to the trapezium bone. The surgeon uses a special tool to hollow out the trapezium bone, removes the cartilage between the two bones, and then uses a pin to connect the two bones together. The pin allows for the bones to stay together or fuse as it heals.
Surgery Considerations
- After surgery, you will no longer have the ability to bend your thumb like you did prior to the surgery
- Surgery failure rate is between 8-21 percent, requiring a surgical revision
- You may lose the ability to place the hand flat on a surface
- Complications like nerve damage can occur
- Rehabilitation will be necessary after surgery to regain range of motion and learn how to protect the thumb joint
- The joint will no longer be painful since it is immobile
Ligament Reconstruction and Tendon Interposition (LRTI)
Who is it for?
LTRI is typically performed on patients with thumb CMC osteoarthritis who have tried other conservative measures but they have failed to manage symptoms.
People with symptomatic CMC OA that affects the ability to pinch, grasp, and grip with the thumb. These symptoms may include pain at the base of the thumb, swelling and stiffness.
What is LRTI?
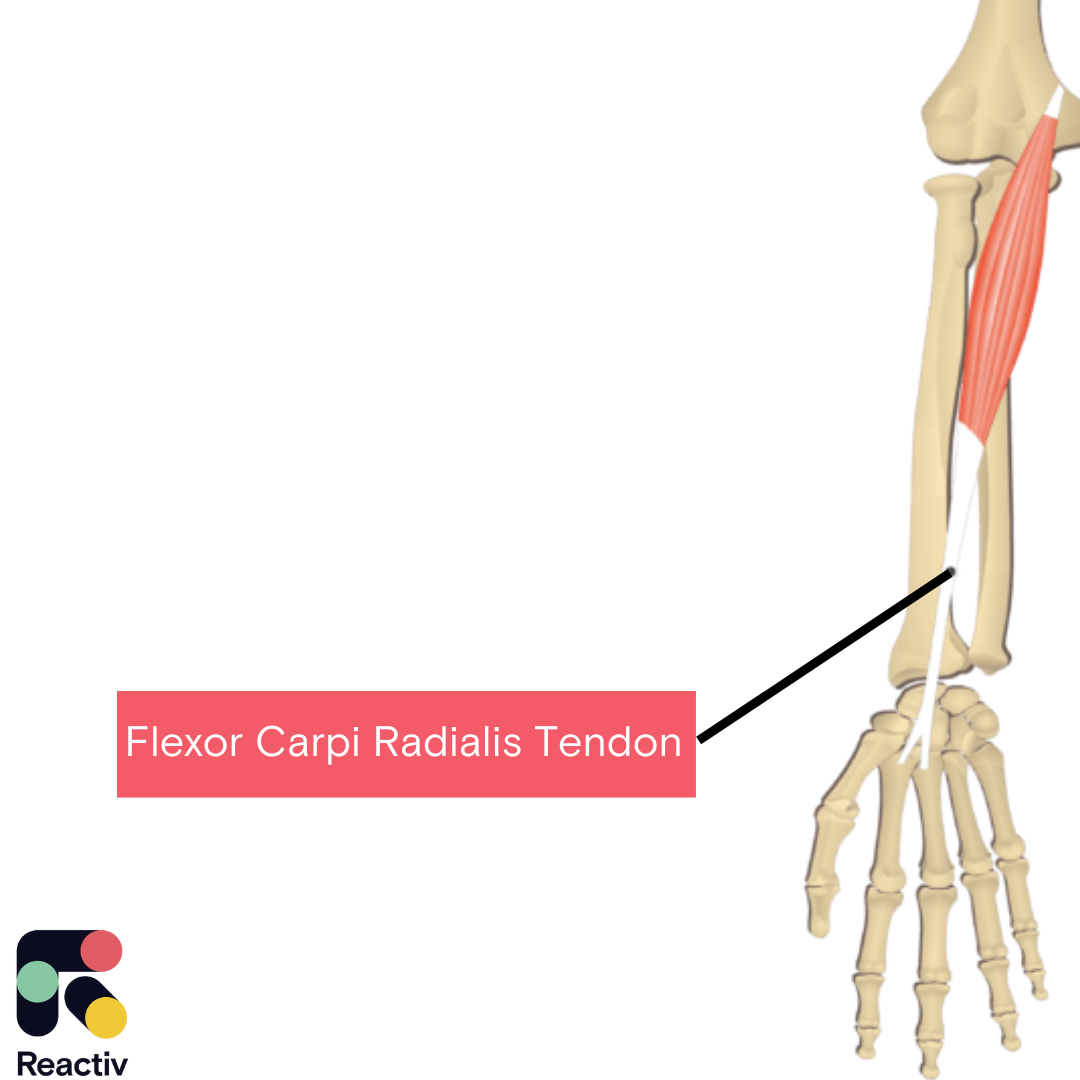
A ligament reconstruction and tendon interposition is a surgical procedure for thumb osteoarthritis that has been used for over 40 years. In this surgery, the surgeon creates a hole in the thumb’s metacarpal bone. A nearby tendon, the flexor carpi radialis (FCR), is passed through the hole in the metacarpal.
The surgeon also removes all or a part of the trapezium bone and the “anchovy” or the remaining part of the tendon is rolled and placed into the space between the bones. This “anchovy” helps to protect the bones from rubbing together and keeps a joint space. In some cases, the “anchovy” may be artificial, eliminating the need to use the remaining tendon to fill the space.
Surgery Considerations
Overall, LRTI has a pretty high success rate at 96%. However, there are some things to consider if you are a candidate for LRTI:
- No two bones are rubbing together, therefore, the arthritis between the joints cannot return.
- The surgery lasts between 15-20 years
- About 4 weeks of wearing a cast after surgery
- May not get full strength back in the thumb
- Requires a lengthy rehabilitation process
- If the surgery fails, there is little revision that can be done since the trapezium bone is removed
- The thumb may appear visually shorter than prior to surgery
Total Joint Arthroplasty
Who is it for?
A total joint arthroplasty for the thumb is performed on patients with thumb CMC arthritis. Specific implants used may be based on joint damage, age, current and desired activity level.
What is total joint arthroplasty?

A total joint arthroplasty or joint replacement is similar to the surgical procedure typically performed on arthritic hips and knee joints. This involves removing part or all of the damaged bone and tissue and replacing it with a prosthetic joint (as seen in the photo). There are different types of replacements used like metal or pyrocarbon.
A total joint arthroplasty or joint replacement is similar to the surgical procedure typically performed on arthritic hips and knee joints. This involves removing part or all of the damaged bone and tissue and replacing it with a prosthetic joint (as seen in the photo above). There are different types of replacements used like metal or pyrocarbon.
The surgeon will first remove the damaged or affected bone/ tissue and then replace it with the prosthetic joint. In some cases a synthetic spacer is placed between the joint whereas in other cases, the tendon is used to cushion between the bones. The exact procedure used is based on each surgeon.
Surgery Considerations
- Total joint replacement typically has a faster recovery and rehabilitation time since it does not require a graft
- Complications exist for use of spacers between the joint like infections
- Total recovery typically takes about 3 months
Trapeziectomy
Who is it for?
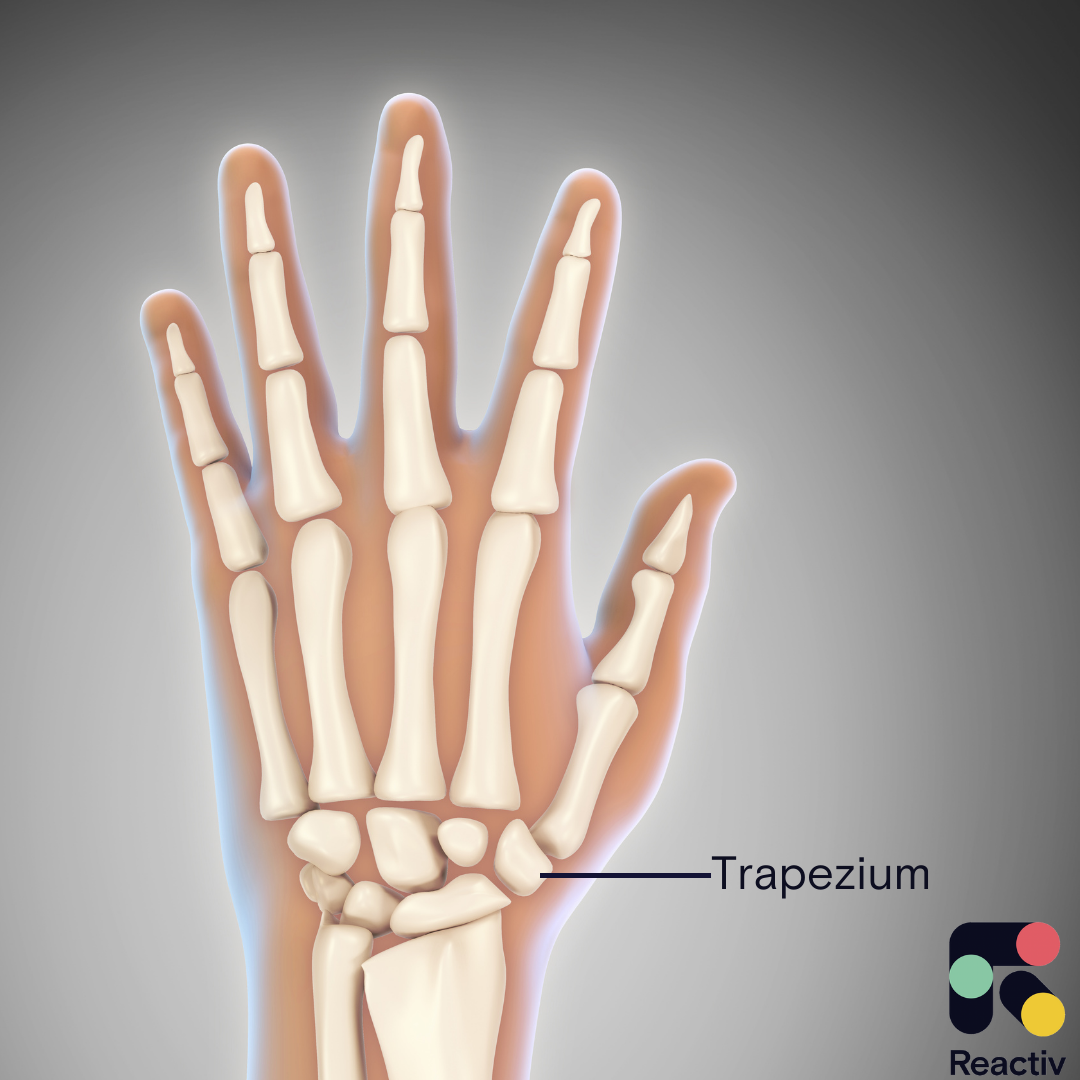
Trapeziectomy involves the surgical removal of the trapezium, the bone that the thumb metacarpal connects.
Trapeziectomies are typically performed on patients with CMC osteoarthritis that have difficulty using the thumb for functional activities.
What is a trapeziectomy?
A trapeziectomy is the complete removal of the carpal bone, the trapezium. Some surgeons will fill the empty space with a folded piece of the tendon or it may be filled with a synthetic spacer.
Surgery Considerations
- There is possibility after surgery for continued thumb pain, nerve damage, scar irritation, swelling, and decreased strength
- Regaining strength and range of motion is possible but may take up to 6 months to achieve
Conclusion:
These surgical procedures are meant to be an overview of some of the most common procedures used to manage thumb arthritis. If you are considering surgery, always consult with your surgeon about which procedure is most beneficial for you and your condition.
Surgical options will depend on your specific condition, pain, disease stage, functional goals, age, and more. They may also depend on the surgeon’s experience, training, and personal preference.
Within each surgical procedure, a surgeon may have a slightly different technique than what is outlined above, which is why it is important to consult with your surgeon about your specific case.
In each case, it is important to listen to your physician both before and after your surgery about recovery timelines and therapy. An important piece of recovery is likely going to be thumb range of motion exercises to build back the strength, motion, and functional use of the hand.
Reactiv built exercises along with occupational therapist to help move your hand and fingers to regain range of motion and gently move your hand.
To give it a try, download the app here:
Reactiv may be covered by your insurance provider. To confirm if you are eligible, please provide your contact details and we will reach out.
